OVERVIEW
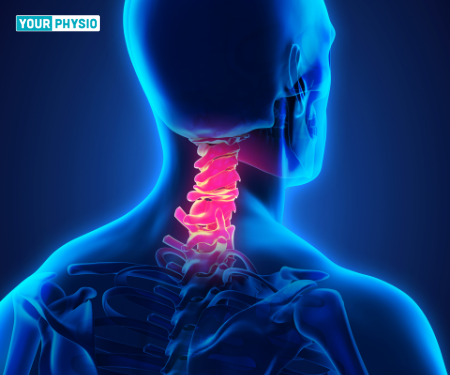
Neck pain can be caused by many things but it is most often related to getting older. Like the rest of the body, the discs and joints in the neck (cervical spine) slowly degenerate as we age.
Cervical spondylosis is also known as arthritis of the neck is the natural wearing down of cartilage, discs, ligaments, bones and joints in the neck that can lead to pain, stiffness and weakness of the neck.
Cervical spondylosis is extremely common. According to studies Cervical spondylosis affects around 85% of adults over the age of 60. Cervical spondylosis was found in 13.76% of the population, however, the proportion varied greatly across urban, suburbs, and rural areas. Changes in the spine are considered a normal part of aging.
The spine likely begins this wearing-down process sometime in your 30s. By age 60, almost nine in 10 people have cervical spondylosis. Furthermore, women had a greater rate i.e. 16.51% more than men which are 10.49%.
CAUSES
1. Degenerated Discs
As the disks in the spine age, they lose height and begin to bulge. They also lose water content, begin to dry out and weaken.
This problem causes settling or collapse of the disc spaces and loss of disc space height which allows more bone-on-bone contact between the vertebrae.
With time, the discs become thinner, and the soft tissue has less elasticity, thus the cushioning qualities of the discs begin to decrease.
2. Herniated Discs
Normal aging can cause part of your spinal disk to tear or crack. This is called a herniated disc.
The herniation can allow the disc to bulge out, pressing on nearby tissue or a spinal nerve.
3. Bone Spurs
The bone tissue rubs directly against other bone tissues when the cartilage in the joints of the vertebrae in the spine begins to degrade.
To make up for the lost cartilage, the body may respond by growing new bone in the joints to help support the vertebrae which result in abnormal bone development around the edges of the vertebrae. This bone growth is called bone spurs or osteophytes.
This may narrow the space for the nerves and spinal cord to pass through. Bone spurs may also lead to decreased range of motion in the spine.
4. Stiff ligaments
Ligaments are cords of tissue that connect bone to bone.
Spinal ligaments can stiffen with age, making your neck less flexible.
5. Osteoarthritis
Osteoarthritis is a progressive (ongoing) condition that causes the cartilage in your joints to degenerate (wear down with time).
With osteoarthritis, cartilage degenerates faster than with normal aging.
Risk Factors
Factors that may increase the risk of developing cervical spondylosis and neck pain include:
Age - This is the most common risk factor for cervical spondylosis. The condition is extremely common in patients who are middle-aged and older.
Genetics -a family history of neck pain and spondylosis
Smoking - It is clearly linked to increased neck pain
Occupation - jobs with lots of repetitive neck motion and overhead work
Depression or anxiety
Previous injury or trauma to the neck
SIGNS & SYMPTOMS
The narrowing of the spinal canal itself does not usually cause any symptoms. It is when inflammation of the nerves occurs at the level of increased pressure that patients begin to experience clinical problems.
For most people, cervical spondylosis causes no symptoms. When symptoms do occur, they typically include,
Neck pain
This may be the main symptom. Pain may get worse when you move the neck.
This pain can range from mild to severe. It is sometimes worsened by activities in which the neck is held in the same position for a prolonged period such as driving or reading a book.
The pain usually improves with rest or lying down
Neck stiffness
Muscle spasms in the neck and shoulders
A nagging soreness in the neck
cracking, clicking, or crunching sound while moving the neck
Headaches.
Lightheadedness
Reduced cervical lordosis ( as the condition progresses)
If the spinal cord or nerve roots become pinched (radiculopathy) the symptoms might include,
Tingling, numbness and weakness in your arms, hands, legs or feet
Lack of coordination and difficulty walking
Loss of bladder or bowel control
DIAGNOSIS
1. Physical examination
After discussing the medical history and general health, your doctor will conduct a thorough examination of your neck, shoulders, arms and, frequently, your legs. They will conduct nu tests, looking for problems or changes in:
The range of motion of the neck and arms
Mobility of your arms, hands, legs and muscle strength
Knot or bump in the shoulder or neck region( tender points)
Strength in your arms, hands, and fingers
Touch sensation
Reflexes
Gait - to check if nerve compression is causing any changes in walk pattern
2. Imaging Tests
Diagnostic tests to help confirm the diagnosis of cervical spondylosis. These tests may include:
X-ray
- X-rays provide images of dense structures, such as bone. An X-ray will show the alignment of the bones along your neck.
- It can also reveal degenerative changes in your cervical spine, such as the loss of disk height or the presence of bone spurs.
MRI
- images show the details of soft tissues such as cartilage, nerve roots, muscles, spinal cord and disks
CT Scan
- provides a clearer picture of the spinal canal and bone spurs.
Myelogram
-In this imaging procedure, contrast dye is injected into the spinal canal to make the spinal cord and nerve roots show up more clearly
Nerve Function Test
- This includes Nerve Conduction Study and Electromyography to determine if nerve signals are travelling properly to your muscles.
Blood tests
- to determine whether a rheumatoid factor or any other antibody indicative of inflammatory arthritis is present.
DIFFERENTIAL DIAGNOSIS
Few other medical conditions that could also include the signs and symptoms of cervical spondylosis are,
Cervical sprain and strain
Cervical myofascial pain
Cervical fracture
Chronic pain syndrome
Fibromyalgia
Adhesive capsulitis
Brachial plexopathy
Thoracic outlet syndrome
Carpal tunnel syndrome
Cubital tunnel syndrome
Multiple sclerosis
Vitamin B12 deficiency
Amyotrophic lateral sclerosis
Guillain-Barre syndrome
Discitis/osteomyelitis
Special Tests For Cervical Spondylosis
1. Spurling’s Test
The traditional Spurling test is done by putting pressure on your head.
You may feel pain or strange sensations. Your doctor will keep the pressure going until the end of the test.
The test will stop sooner if you feel pain or discomfort. If you start to hurt or feel numb, or tingling, or any other sensation radiating down your arm, then you have a positive test.
If you don’t feel any pain during the basic compression test, your doctor will pull your neck to one side and move your head downward.
Then your doctor will rotate your head from side to side, while your head is still extended and facing downward.
You’ll do these movements until you feel pain. If you complete the test and feel no pain, you'll get a negative test result.
2. Neck Distraction test
For this test, your doctor will apply force while grabbing your head under your chin.
You’ll get a positive result if you feel relief in your neck.
3. L’hermitte’s sign
This test works when your doctor flexes your cervical spine.
If you feel a shock-like pain or feeling down your spine or arms and legs, you’ll get a positive test.
4. Hoffman’s sign
Your doctor will have you snap your thumb and index finger.
You get a positive result if your thumb and index finger don't respond to the test, or can't make the movements.
TREATMENT
In most cases, cervical spondylosis responds well to conservative treatment that includes medication and physical therapy.
The treatment strategy for cervical spondylosis depends on the severity of a patient’s signs and symptoms. In the absence of “red flag” symptoms the goals of treatment are to relieve pain, improve functional ability in day-to-day activities, and prevent permanent injury to neural structures. Symptomatic cervical spondylosis should be approached in a stepwise fashion, starting with non-operative management.
The conservative management (non-surgical) for cervical spondylosis is as follows,
1. Medications:
medicines including nonsteroidal anti-inflammatory drugs (NSAIDs), oral steroids or injections, muscle relaxants, anticonvulsants, antidepressants and opioids are the preferred drug groups for pain relief.
2. Physiotherapy:
The mainstay of non-surgical treatment is a four- to six-week course of physical therapy.
Immobilisation of the cervical spine plays a major role in conservative treatment for patients with cervical spondylosis by limiting the motion of the neck, thereby reducing nerve irritation
Supportive devices
- Based on the patient's tolerance and compliance, soft cervical collars are recommended for daytime use only as it allows rest and support to muscles and joints.
- More rigid orthoses (eg, Philadelphia collar, Minerva body jacket) can significantly immobilise the cervical spine.
- However, a neck brace should be worn for only short periods because it can eventually weaken neck muscles.
Physiotherapy techniques
- Techniques like manipulation and soft tissue mobilisationcan be used to reduce pain, improve function and increase the range of motion.
Postural education
- Includes the alignment of the spine during sitting and standing activities
- Moulded cervical pillows can better align the spine during sleep and provide symptomatic relief for some patients.
Devices
- Electrical devices like IFT, ultrasound and TENS can be used for acute pain relief but needs to be combined with exercises after the usage of these devices.
- Mechanical traction is a widely used technique. It helps in promoting immobilisation of the cervical region and widens the foraminal openings.
Exercises
Exercises should include
- Stretches: improves neck and upper back flexibility
- range of motion exercises: to maintain and improve neck range and to prevent stiffness
- strengthening exercises: Isometric and resistance exercises are often beneficial to maintain the strength of the neck muscles.
- proprioceptive reeducation exercises
3. Education.
Patient education plays a vital role in cervical spondylosis management therefore the following information should be reinforced.
The natural history of cervical spondylosis is highly variable, as well as challenging to prevent, given that it is part of the normal aging process.
The client should receive training on ways to deter the early onset of cervical spondylosis, including maintaining good neck strength and flexibility, leading an active and healthy lifestyle,
Prevention of neck injuries (e.g., good ergonomics, avoiding prolonged neck extension, proper equipment for contact sports, safe tackling technique, and seatbelt use in automobiles)
Avoid high-impact exercise (eg, running, jumping)
Apply heat or ice typically no more than 20 minutes at a time, several times a day.
Surgical Management
Surgical intervention should be considered in patients with severe or progressive cervical myelopathy, following the failure of above mentioned non-surgical measures.
Few surgical interventions are partial discectomy, laminotomy-foraminotomy, laminoplasty, and laminectomy based on anterior or posterior approach.
Conclusion
Cervical spondylosis is considered a natural process of aging with a 95% prevalence by age 65 years. Most people remain asymptomatic but can present with neck pain, as well as progress to cervical radiculopathy and/or cervical myelopathy.
Cervical Spondylosis can be painful and can hinder daily activities. Severe symptoms might require surgery or medication but the initial stage symptoms can easily get treated with early diagnosis and exercise protocol. A physiotherapist can help you in creating an exercise regimen with proper guidance thus helping ineffective management of cervical spondylosis.
Take an online physiotherapy consultation today to learn more about the treatment procedures for cervical spondylosis: On a mission to make people's lives pain free - YourPhysio
Illustrations designed by freepik